Senators Slam Private Equity–Fueled Hospital Giant in Charged Hearing
In front of a packed room at a Senate hearing on Thursday, longtime nurse Ellen MacInnis recounted working at a Massachusetts hospital owned by Steward Health Care, the nation’s largest for-profit hospital provider. Her voice broke as she remembered the many times she and her colleagues couldn’t give their patients the very best care because Steward insisted on saving money: by laying off staff, cutting resources, and leaving medical supply bills unpaid.
During one shift, MacInnis remembered, there were 95 patients in the emergency room and only 11 nurses; that day, she said, an elderly man awaiting chemotherapy treatment suddenly died in the ER. Another day, a patient in mental health crisis arrived in the emergency room. Without enough staff, they couldn’t allocate someone to watch him continuously, as is standard procedure. That patient went into distress and died.
The veteran nurse told this story in front of the Senate Committee on Health, Education, Labor, and Pensions (HELP), which held a charged hearing on the abuses of Steward and its investor owners. In response to testimony from MacInnis and others about the abysmal patient treatment they witnessed thanks to Steward’s extractive business model, lawmakers from both sides of the aisle assailed the company and promised to work on legislation to prevent Wall Street firms from looting hospital systems, amid a growing trend of private equity investment in health care.
“The collapse of Steward Health Care is just one extreme example of the damaging role that private equity is having, in my view, on our health care system.”
“Private equity firms have bought up hundreds of hospitals, thousands of nursings homes, and tens of thousands of medical practices,” said Sen. Bernie Sanders (I-Vt.) in kicking off the hearing. “The collapse of Steward Health Care is just one extreme example of the damaging role that private equity is having, in my view, on our health care system.”
Steward declared bankruptcy in May, and has come under fire this year as details have emerged about the many ways the company prioritized enriching its top brass and investors at the expense of patient care, eventually running the chain into financial ruin. The company, which operates hospitals in eight states, was formed when private equity firm Cerberus bought a Massachusetts Catholic hospital chain in 2010, and is now owned by a publicly traded real estate investment trust (REIT) called Medical Properties Trust.
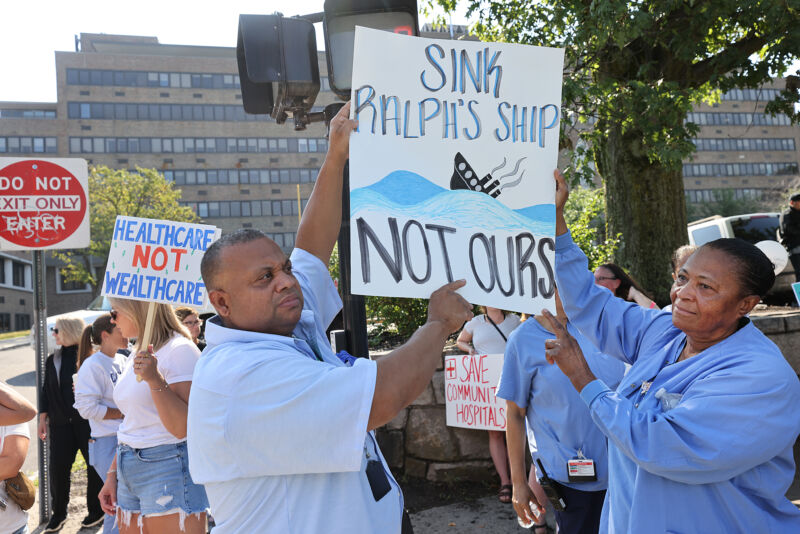
A recent Boston Globe investigation revealed that Steward’s disinvestment in patient care led to at least 15 deaths over the past 14 years. At the same time, top executives at Steward earned enormous sums while cutting costs at their hospitals, placing strain on health care providers trying to do their jobs and leading to subpar care for patients. In particular, Steward CEO Ralph de la Torre—who bought a $40 million yacht and a $15 million luxury fishing boat, uses two private jets Steward purchased for a combined $95 million, and who received a $100 million dividend when he engineered the sale of Steward to MPT—has drawn sharp criticism from the likes of Sanders and Sen. Elizabeth Warren (D-Mass.).
De la Torre was subpoenaed to appear before the Senate HELP Committee in July. About a week ago, his attorneys informed the committee that he was planning to defy the subpoena. On Thursday, committee members announced they would file resolutions to hold de la Torre in contempt for refusing to show. If he is prosecuted and convicted of criminal contempt, de la Torre could face a fine of up to $100,000 and jail time.
“The corporatization and commodification of hospital care has led to horrific harm and suffering to our patients.”
At Thursday’s hearing, nurse Audra Sprague recounted how the beds at her hospital would not be repaired when they broke. Staff then rented beds to fill in the gap. But Steward stopped paying the rental bed vendor, forcing Sprague and her colleagues to transfer patients to other hospitals because they didn’t have a physical place for them to lie. Her hospital, which served a rural population in central Massachusetts, closed abruptly last month due to Steward’s bankruptcy. It was licensed for 57 beds, but Sprague said that by the time it closed there were only 18 working ones left.
MacInnis added that Steward’s habit of understaffing their hospitals, as well as failing to pay many vendors, led to preventable patient harm and death. “The immediate and most debilitating impact of the ownership of Steward was Steward’s tendency to understaff units whenever and wherever they can,” she said. “The corporatization and commodification of hospital care has led to horrific harm and suffering to our patients.”
Throughout the hearing, lawmakers asked witnesses what sort of regulation they believed would help prevent more Stewards in the future. The mayor of West Monroe, Louisiana, Staci Mitchell, agreed that greater transparency into the opaque actions and finances of private equity and REIT hospital owners could have helped prevent some of the harms that unfolded at the Steward hospital in her community, Glenwood Medical Center, which included a major reduction in emergency services, layoffs of hundreds of medical staff, and strain on small businesses in the community who were owed tens of thousands by Steward for work.
After the hearing, Sen. Ed Markey (D-Mass.) held a press conference where he shed further light on lawmakers’ plans to try to regulate private equity purchases of hospitals with the Health Over Wealth Act. Introduced this summer, the bill would require that private equity–owned health care providers publicly report their debt, executive pay, health care costs charged to patients, and any reductions in services to patients or to staff pay—the kind of transparency that might help spot the sort of drastic cost-cutting that Steward Health Care engaged in for years.
The bill “will ensure transparency, accountability, protections for patients and providers, and guarantee access to care for every community in the country,” Markey said in a statement. “I am committed to preventing Steward’s failures from becoming America’s health care standard.”